1 in 4 young adults in Singapore reported poor mental health in 2024, the highest among all age groups surveyed
Summary
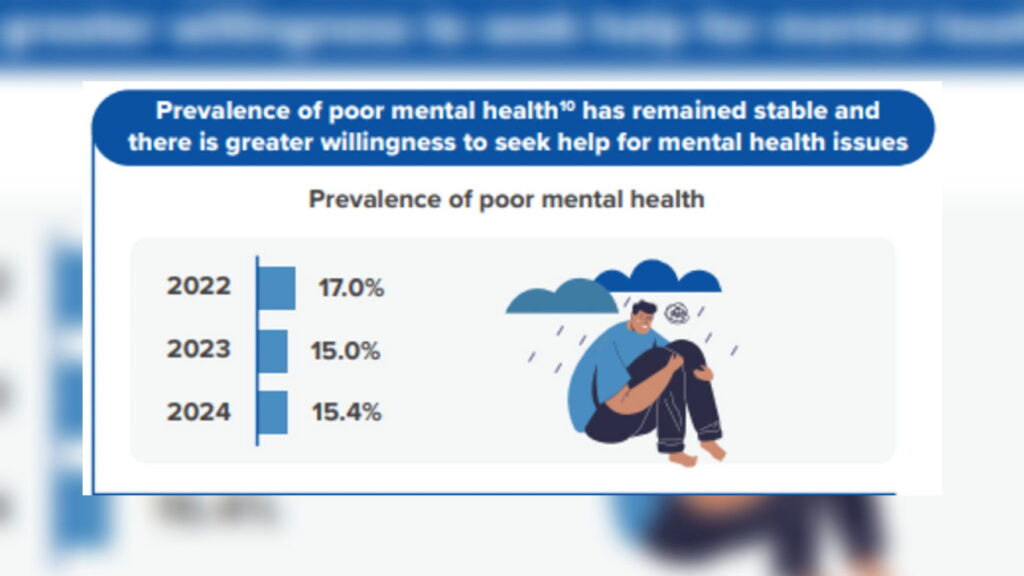
The National Population Health Survey (NPHS) 2024 used the 12-item General Health Questionnaire (GHQ-12) with a cut-off score of 3+ to measure poor mental health. Overall, 15.4% of Singapore residents aged 18–74 were classified as having poor mental health in 2024. The rate was highest among young adults (18–29) at 25.5%, and particularly high for young females in that group (31.7%). Females overall reported poorer mental health than males (17.3% vs 13.5%).
Rates varied by ethnicity and education: Indians (18.0%) and Malays (17.7%) had higher prevalences than Chinese (15.1%), and residents with post-secondary education reported higher prevalence (16.7%) than those with primary or secondary education. When stressed, most residents preferred seeking help informally from friends and family (81.8%) rather than from healthcare professionals (64.0%).
On the positive side, the NPHS found improving health behaviours: sufficient total physical activity returned to pre-COVID levels, influenza and pneumococcal vaccination uptake rose, and daily smoking reached an all-time low. However, chronic conditions remain common (about one in three have hyperlipidaemia or hypertension) and obesity increased from 10.5% (2019–2020) to 12.7% (2023–2024). The government has expanded mental-health access via First Stops for Mental Health and the round-the-clock mindline 1771 helpline (launched June 2025), plus awareness and peer-support programmes.
Key Points
- Overall prevalence of poor mental health (GHQ-12 ≥3) among 18–74 year-olds: 15.4% in 2024.
- Young adults (18–29) show the highest rate at 25.5%; young females in this group: 31.7%.
- Females report higher poor mental health than males (17.3% vs 13.5%).
- Higher prevalences observed among Indians (18.0%) and Malays (17.7%) compared to Chinese (15.1%).
- Residents with post-secondary education had a higher prevalence (16.7%) than those with lower education levels.
- Preference for informal help is strong (81.8%) versus healthcare professionals (64.0%); willingness to seek help falls with age.
- Health behaviours improving: physical activity and vaccination rates up, smoking down; but obesity is rising and chronic disease prevalence remains substantial.
- Policy response includes First Stops for Mental Health and the national mindline 1771 helpline to improve access and support.
Context and relevance
These findings matter for employers, HR teams, policymakers and health services. A high burden of poor mental health among younger adults affects productivity, talent retention and workplace wellbeing strategies. The preference for informal support suggests stigma or barriers to clinical care remain, even as uptake of preventative health measures improves. Rising obesity alongside persistent chronic disease prevalence points to continuing public-health challenges requiring integrated prevention and support programmes.
Why should I read this?
Because one in four young people struggling is not a marginal stat — it’s a red flag. If you manage people, design benefits or shape workplace wellbeing, this short read gives you the key numbers and what’s changing fast. We’ve done the heavy lifting so you can act quicker.